
KX exceptions and Medicare Payment Reductions for 2019
Last Friday we heard about three changes:
- The KX exception (for use when treatment above the $2,010 cap can be defended) has been continued, indefinitely.
- The $3,600 Medicare “Threshold” has been reduced to $3,000.
- In 2022, CMS will lower PTA and COTA reimbursements by 15%.
Beyond these high-profile changes, something else is new:
The Medicare Payment Reduction You Didn’t Hear About
For treatments as of January 1, 2018, Medicare has lowered reimbursements on some of the most widely-used CPT codes in outpatient rehab.
Offsetting these reductions, reimbursements for five other CPT codes have been increased. (Refer to your MAC’s fee schedule for details).
Cut
Therapeutic Exercise (97110) – 5% cut
Manual Therapy (97140) – 6.6% cut
Aquatic Therapy (97113) – 9% cut
Increased
Massage (97124) – 19.3% increase
Therapeutic Activities (97530) – 17.3% increase
Electrical Stimulation (G0283) – 8.9% increase
Ultrasound (97035) – 6.5% increase
Neuromuscular Re-education (97112) – 3.7% increase
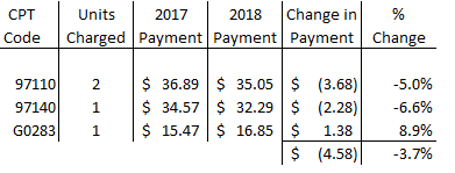
If you are a typical practice that charges Medicare “2 Ther-Ex, 1 Manual and 1 E*Stim”,
on average you’ll suffer a 3.7% pay cut. $4.58 lower reimbursements.
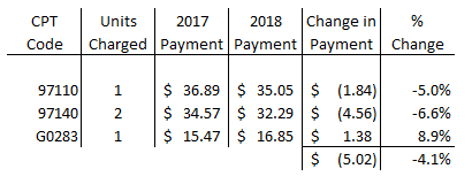
If you typically charge Medicare “1 Ther-Ex, 2 Manual and 1 E*Stim”,
the average pay cut will be 4.1% pay cut. $5.02 lower reimbursements.
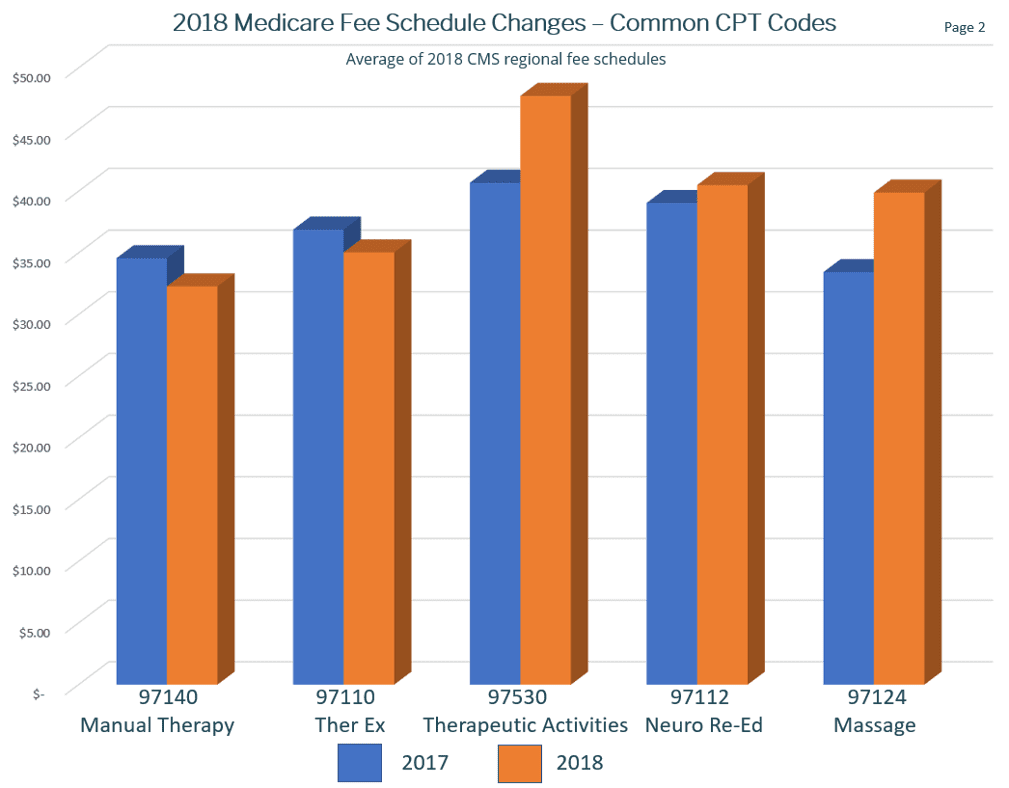
Reviewing changes to Medicare’s fee schedule on a graph may shed insight into how to offset lower fees. Blue columns are 2017 reimbursement rates, Orange are 2018. Notice Therapeutic Activities vs. Ther-Ex. As CMS is apparently placing a higher value on activity-based / function-oriented care, many practice owners are reconsidering their approach to treatment. Example, rather than increasing shoulder/arm strength and ROM with Ther-Ex, some practices are further enhancing treatment toward restoring the reported functional deficit, (ex. lifting/carrying items)and as such, legitimately charge for Therapeutic Activities. Orienting the treatment plan more precisely toward restoration of the identified deficit (and thoroughly defending it as such in your documentation) results in a more function-based treatment plan as well as higher reimbursements.
Our industry is fluid. As the pace of change accelerates:
- Keep aware of changes
- Be open to new approaches (don’t get stuck in yesterday’s approaches)
- Innovate new ways to orient treatment more and more toward functional restoration
- Superior patient progression combined with higher reimbursements are a win-win

