The Fastest EMR for Physical Therapy
Electronic Medical Record – EMR
Over the past two decades, SYSTEMS4PT has reinvented physical therapy EMR software. Our approach is unique, like nothing you’ve seen before. Purpose-built documentation made for Physical Therapists like you, will solve your clinic’s biggest problems.
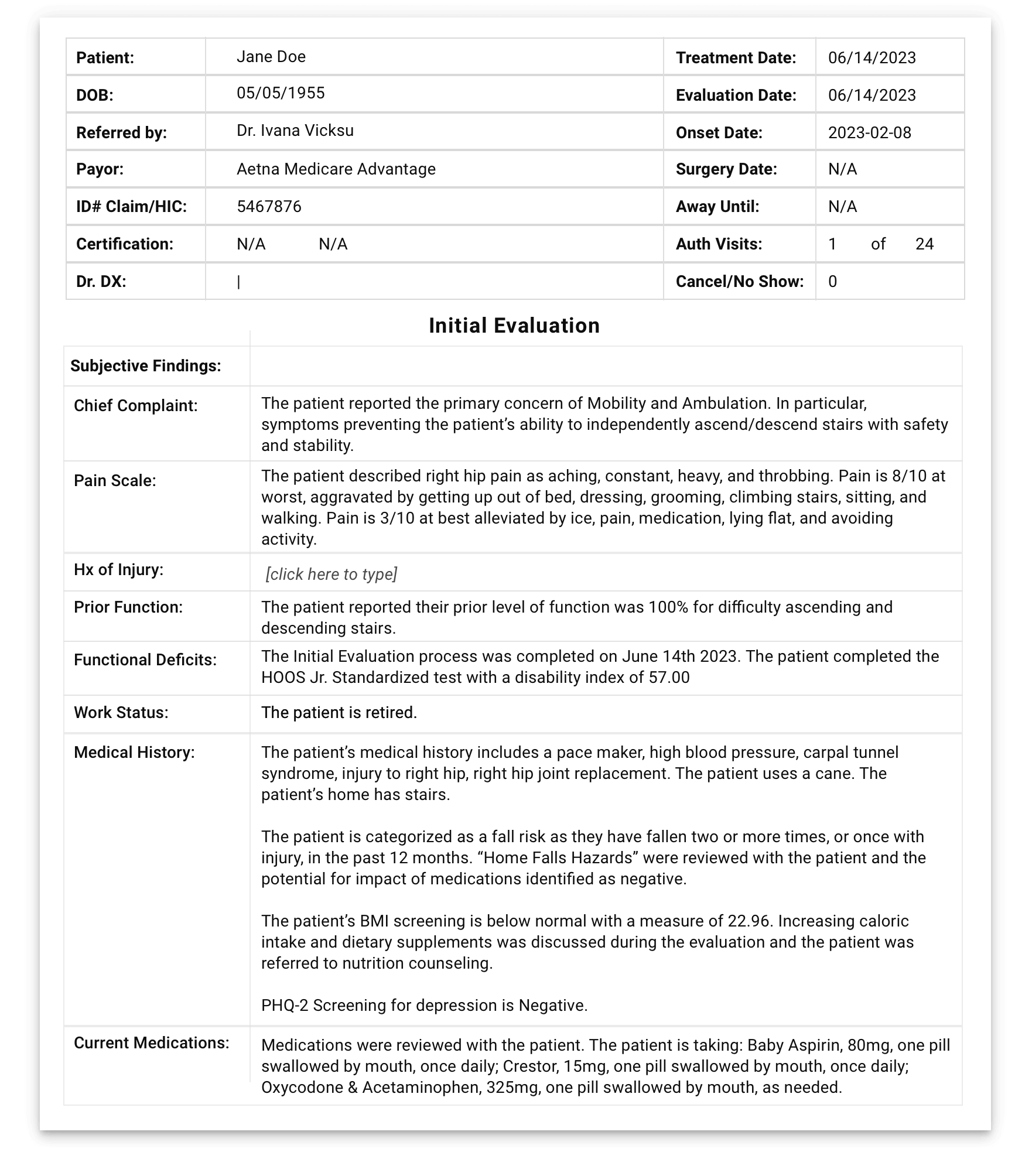
Evaluation
The evaluation process begins with our EMR-integrated Patient Intake Portal,
With APTA & Medicare approved Functional Outcome Tests & medical history forms, patients can receive intake and assessment forms before their appointment through a secure link sent to their email or cell phone or complete forms at the appointment using a desktop or mobile device.
Our system data mines the intake results, building, on average, 1,250 words of defensible documentation demonstrating medical necessity. Next, the documentation then populates your fully interactive evaluation template with the following information:
- Patient account details
- Medical history & current medications
- The patient’s work, school, and living status
- The patient’s chief complaint & concerns
- Patient pain scale rating results
- Prior level of functionality
- Functional Outcome Test type, date, & disability index score
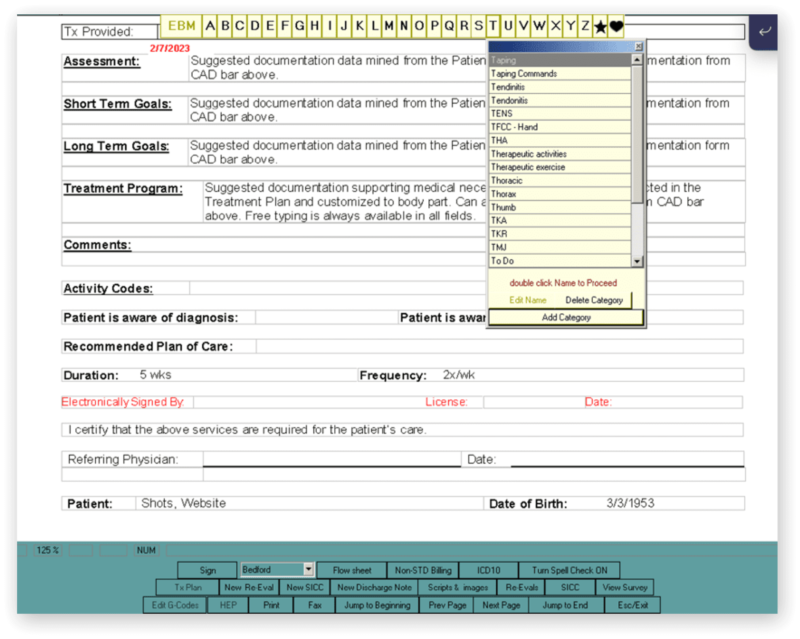
Finally, document deficits, goals, and treatment plans with just a few clicks using our Computer Assisted Documentation and Treatment Plan Library with built-in CPT codes!
EMR with Smart Documentation, Simplifying Patient Record-Keeping
Systems4PT identifies key patient information and captures that data automatically.
After intake, your patient’s demographics, medical history, billing information, and details about their condition, functional assessment findings, and therapy goals are available in your evaluation documentation.
Systems4PT’s EMR provides you with a library of industry-standard treatment plan templates. Our templates populate clean CPT codes auto-fill with maximum, legitimate charge capture, all satisfying Medicare’s 8-minute rule and other common payor regulations.
Our custom CAD (Computer Aided Documentation) Bar helps you document in half the time compared to other EMRs. Enter measurements, objective findings, and short-term and long-term goals in seconds with our Rapid-Fire-Entry feature.
Additionally, our built-in Medicare compliance control systems ensure your Progress reports are completed at least once every 10 treatment days/30 calendar days.
Daily Notes
Our EMR for physical therapy is centered around compliance and built to help you spend less time at your computer and more time treating patients. Take the repetitiveness out of Daily Notes and start documenting quickly and confidently with the following features:
- Forward transfer of subjective and objective data from previous encounter
- Pre-loaded evidence-based treatment templates & smart flowsheet template
- Auto-recommend charges based on the 8-minute rule
- Authorized visits and script tracking show when a progress note or new authorization is due
- Fax directly from patient notes to the referring physician
- Seamless navigation through patient records
Review your notes, update as needed, and track progression through treatment before the patient leaves your practice. Twice the compliance – half the time with Systems4PT’s EMR for PT.